Otomastoiditis: a rare form of extrapulmonary tuberculosis
DOI:
https://doi.org/10.5935/2764-734X.e20240946Keywords:
Tuberculosis Extrapulmonary;, Otitis Media with Effusion, Tuberculosis, Pulmonary, Mastoiditis, Case ReportsAbstract
Although predominantly associated with pulmonary manifestations, tuberculous otitis media is a rare clinical manifestation of extrapulmonary dissemination. This case report presents a 41-year-old patient with HIV/AIDS who developed otalgia, otorrhea, cough, and dyspnea 10 days after being physically assaulted. He was admitted with pulmonary sepsis, and the presence of Mycobacterium tuberculosis in his sputum was identified by rapid molecular testing on the second day of hospitalization. A computed tomography (CT) scan of the skull revealed mastoiditis on the right (no bone lesion), and ear secretion also confirmed the tuberculous etiology. The patient satisfactorily responded to the specific treatment.
Downloads
INTRODUCTION
Tuberculosis (TB), an infectious disease caused by the bacterium Mycobacterium tuberculosis, remains a major health threat in Brazil and worldwide1-3. Although predominantly associated with pulmonary manifestations, tuberculosis can spread to other organ systems, tuberculous otitis media (TOM) being a rare manifestation of extrapulmonary tuberculosis4,5. TOM accounts for between 0.05% and 0.9% of cases of chronic otitis media5, often leading to late diagnosis because it is rarely considered in the differential diagnosis4,6-8.
The medical literature on TOM in adults is scarce, and it mainly comprises isolated case reports or limited series9. This case report presents a clinical example of TOM in an adult patient and contextualizes this rare manifestation within the broad spectrum of extrapulmonary tuberculosis.
CASE REPORT
A 41-year-old man sought emergency medical care with a history of having suffered physical aggression through bodily force in both ears 10 days previously, followed by otalgia and purulent secretion from the right ear associated with hyporexia. After 6 days, he began to present with productive cough, dyspnea, unmeasured fever, and nausea. On the day before admission, he experienced an episode of “convulsion” (sic). He also reported losing 20kg in the last 2 months.
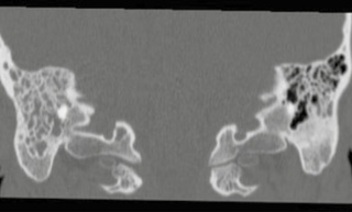
The patient had been aware that he was positive for HIV since 2014 but denied any previous opportunistic infections or hospitalizations, despite being poorly adherent to antiretroviral therapy. On admission, his general state was regular, hypotensive, and tachycardic; the sepsis care protocol was immediately started with antibiotic therapy (ceftriaxone) directed at the pulmonary focus. The patient was referred to the intensive care unit (ICU) for ventilatory and hemodynamic support, where he was given a non-rebreathing mask and vasoactive drugs, without the need for invasive ventilation. Because of his respiratory condition and history of seizures, he was referred for computed tomography (CT) scans of the skull and chest. CT scan of the skull revealed signs of mastoiditis on the right (Figures 1 and 2) without bone erosion, while the hypothesis of meningoencephalitis was ruled out by normal analysis of the cerebrospinal fluid. Chest CT revealed ground-glass opacities and others with a “sprouting tree” pattern bilaterally, as well as bronchial thickening and more marked consolidative areas in the right lung, with a small cavity in the middle lobe. Considering the patient’s pulmonary condition and history of irregular treatment for HIV infection, sputum was collected, and the rapid molecular test results for Mycobacterium tuberculosis were positive and sensitive to rifampicin.
Figure 1. TCT-scan of the skull with a coronal view of the mastoids. Non-cholesteatomatous mastoiditis on the right, without bone erosion.
Figure 2. A and B. Axial view in CT-scan of the skull. Mastoid veiling is shown on the right.
Specific treatment with rifampicin, isoniazid, pyridoxine, and ethambutol (RIPE) was started on the third day of hospitalization, and ceftriaxone was continued for a further 9 days. He improved satisfactorily and was discharged from the ICU on the fifth day of hospitalization. He was already off vasoactive drugs and oxygen supplementation, but otorrhea persisted. The otorhinolaryngology (ENT) team was asked to evaluate the case and collected a secretion from the right ear, which was also positive for M. tuberculosis and rifampicin-sensitive. On the 15th day of hospitalization (the 12th day of treatment with RIPE), he was discharged (without otalgia and otorrhea) for specialized follow-up with ENT (among others, for audiological assessment) and infectology, as well as being referred to the Basic Health Unit to receive supervised treatment for tuberculosis (initially for the usual period of 6 months, depending on clinical progress). The laboratory results available only after hospital discharge included a serum CD4 cell count of 20/µL, a viral load of 90,054 copies/mL (tests collected on admission), and the growth of Mycobacterium tuberculosis in the sputum culture but not in the ear secretion (there was contamination) or cerebrospinal fluid (negative culture).
DISCUSSION
The analysis of this case report offers valuable insights into the atypical clinical presentation and the diagnostic hypothesis based on a history of recent trauma. The physical aggression preceding otalgia and purulent otorrhea led clinical reasoning in favor of a nonspecific bacterial infection as the first diagnostic hypothesis, possibly even associated with a more serious bone lesion. However, given the mastoiditis observed on the skull CT scan-with no fractures identified-and the confirmed diagnosis of pulmonary tuberculosis in a patient positive for HIV, extrapulmonary tuberculosis emerges as a possible complication of the trauma, as previously described in relation to the auricular region, although rare7. The classic triad of TOM is painless otorrhea, multiple perforations of the tympanic membrane, and facial paralysis4,7-9, and our patient experienced only painful otorrhea.
CT revealed signs of mastoiditis consistent with the radiological findings of similar cases3,6,9,10. Otomastoiditis is a suppurative infection of the mastoid cells that usually occurs as a consequence of acute otitis media and can lead to complications, such as hearing dysfunction, facial nerve paralysis, thrombophlebitis, labyrinthitis, osteomyelitis, brain abscesses, meningitis, sepsis, and death8-10. In this context, tuberculous otomastoiditis can present with signs and symptoms similar to nontuberculous otitis media, which often delays diagnosis.
A possible complication of TOM is progressive hearing loss due to perforations of the tympanic membrane, which is usually discreet at the onset of the condition and may be underestimated2,10,11. The case evolved satisfactorily with an evident good response to the specific treatment (RIPE); however, the patient was referred for specialized follow-up by the ENT team.
The usual drug treatment for tuberculosis (RIPE) is sufficient for most cases of TOM. Sensitivity to rifampicin-as detected by molecular biology tests conducted on our patient-infers greater compliance and better prognosis2. However, a possible surgical approach should be considered for the following indications: obtain a histological sample for diagnostic purposes, drain a subperiosteal abscess, remove bone sequestration, and, in select cases, decompress the facial nerve6.
CONCLUSION
This case illustrates the importance of including tuberculous otomastoiditis in the diagnostic hypotheses for otitis media in immunosuppressed patients, even in the face of an obvious cause (trauma, for example) and regardless of the response to nonspecific treatment. In this context, the multidisciplinary approach and the concomitant diagnosis of pulmonary tuberculosis in our patient certainly contributed to the successful outcome.
“This case report deserved an official declaration of acknowledgement and ethical approval by its institution of origin and was peer-reviewed before publication, whilst the authors declare no fundings nor any conflicts of interest concerning this paper. It is noteworthy that case reports provide a valuable learning resource for the scientific community but should not be used in isolation to guide diagnostic or treatment choices in practical care or health policies. This Open Access article is distributed under the terms of the Creative Commons Attribution License (CC-BY), which allows immediate and free access to the work and permits users to read, download, copy, distribute, print, search, link and crawl it for indexing, or use it for any other lawful purpose without asking prior permission from the publisher or the author, provided the original work and authorship are properly cited.”
References
1. World Health Organization (WHO). Global tuberculosis report 2023 [Internet]. Geneva: WHO; 2023; [acesso em 2024 Mai 25]. Disponível em: https://iris.who.int/bitstream/handle/10665/373828/9789240083851-eng.pdf?sequence=1
2. Pai KK, Omiunu AO, Peddu DK, Au VH, Baredes S, Jyung RW, et al. Tuberculosis of the middle ear: a systematic review. Am J Otolaryngol. 2022;43(5):103571. DOI: 10.1016/j.amjoto.2022.103571
3. Cao T, Liu X, Yang C, Mei C, Ou J, Du R. Multidrug-resistant tuberculosis in middle ear: a case report. J Clin Tuberc Other Mycobact Dis. 2023;31:100355. DOI: 10.1016/j.jctube.2023.100355
4. Deenadayal DS, Kumar BN, Bommakanti V, Sameeri KL. Tuberculous otitis media - a rare entity or a missed diagnosis. Int J Otolaryngol Head Neck Surg. 2016;5(02):65. DOI: 10.4236/ijohns.2016.52011
5. Sens PM, Almeida CI, Valle LO, Costa LH, Angeli ML. Tuberculosis of the ear, a professional disease? Braz J Otorhinolaryngol. 2008;74(4):621-7. DOI: 10.1016/s1808-8694(15)30614-5
6. Saunders NC, Albert DM. Tuberculous mastoiditis: When is surgery indicated? Int J Pediatr Otorhinolaryngol. 2002;65(1):59-63. DOI: 10.1016/s0165-5876(02)00121-0
7. Singh A, Irugu DV, Verma H, Thakar A. Atypical presentation of aural tuberculosis with complication. BMJ Case Rep. 2018;2018:bcr-2017-222482. DOI: 10.1136/bcr-2017-222482
8. Dale OT, Clarke AR, Drysdale AJ. Challenges encountered in the diagnosis of tuberculous otitis media: case report and literature review. J Laryngol Otol. 2011;125(7):738-40. DOI: 10.1017/S0022215111000971
9. Sebastian SK, Singhal A, Sharma A, Doloi P. Tuberculous otitis media - series of 10 cases. J Otology. 2020;15(3):95-8. DOI: 10.1016/j.joto.2019.12.001
10. Salata TM, Ribeiro BN, Muniz BC, Antunes LO, Rosas HB, Marchiori E. Distúrbios da audição - achados na tomografia computadorizada e ressonância magnética: ensaio iconográfico. Radiol Bras. 2018;52:54-9. DOI: 10.1590/0100-3984.2016.0213
11. Rubio JMD, Alarcon AV, Palma DM, Vales O, Hinojosa R, Morales DJ, et al. Neuro-otologic manifestations of tuberculosis: "the great imitator." Am J Otolaryngol. 2015;36(3):467-71. DOI: 10.1016/j.amjoto.2015.01.018
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Infections in Evidence

This work is licensed under a Creative Commons Attribution 4.0 International License.
The Copyright Transfer Agreement also understands that the authors guarantee that the respective Case Report has never been published in another communication vehicle or scientific journal. Papers presented at meetings and/or scientific congresses may be published in the electronic Journal INFECTIONS IN EVIDENCE - Case Reports, provided they have not been published in whole or in part in their Proceedings or Annals in the format of a complete article including images, discussion and bibliographic references, or that they have not been assigned a specific DOI number.
















