Paradoxical reaction during treatment of spinal tuberculosis in an immunocompetent individual
DOI:
https://doi.org/10.5935/2764-734X.e20250461Keywords:
Spinal Tuberculosis, Discitis, Antituberculosis Agents, Case ReportAbstract
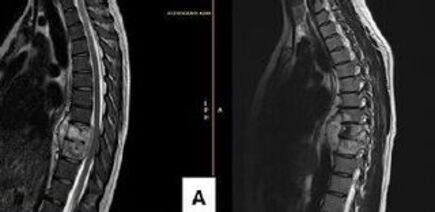
Paradoxical reactions to the treatment of spinal tuberculosis in HIV-uninfected individuals, with clinical and radiological worsening, are rarely described in the literature. We report the case of a 26-year-old woman complaining of pain in the thoracic spine who had a previous history of coughing, night sweats, and weight loss. Magnetic resonance imaging of the thoracic spine showed discitis and incipient spinal cord compression. Despite the negative results of the etiological investigation, empirical treatment for tuberculosis was initiated based on clinical and radiological criteria. Despite adequate medication, the patient developed alterations in physical examination suggestive of spinal cord compression, which was also observed on new imaging findings of worsening bone involvement, deformity of the vertebral bodies, and increased adjacent fluid collections. Consequently, a surgical approach with resection of the posterior vertebral element and arthrodesis was necessary, and the diagnosis was confirmed by a rapid test for tuberculosis using a sample taken intraoperatively. The patient progressed satisfactorily without sequelae during the drug treatment period, which did not include corticosteroids.
Downloads
References
Im JH, Baek JH, Kwon HY, Lee JS. Paradoxical reaction of tuberculous vertebral osteomyelitis: a case series. Infect Dis (Lond). 2015 Apr;47(4):271-4. DOI: 10.3109/00365548.2014.990508
Robledo-Gil T, Harada K, Ikuta I, Villanueva M. Paradoxical Reaction in a Patient with Co-Occurring Tuberculous Meningitis and Pott’s Disease. Am J Case Rep. 2018 Jun;19:699-704. DOI: 10.12659/AJCR.909194
Cheng VC, Ho PL, Lee RA, Chan KS, Chan KK, Woo PC, et al. Clinical spectrum of paradoxical deterioration during antituberculosis therapy in non-HIV-infected patients. Eur J Clin Microbiol Infect Dis. 2002 Nov;21(11):803-9. DOI: 10.1007/s10096-002-0821-2
George AJ, Santhanagopal S, Mohan MM, Lal JV, Basappa M, Thomas JC, et al. Spondylodiscitis: A Diagnostic and Management Dilemma. Cureus. 2024 Apr 15;16(4):e58284. DOI: 10.7759/cureus.58284
Ling-Shan C, Zheng-Qiu Z, Jing L, Rui Z, Li-Fang L, Zhi-Tao W, et al. Magnetic resonance imaging features for differentiating tuberculous from pyogenic spondylitis: a meta-analysis. Skeletal Radiol. 2024 Apr;53(4):697-707. DOI: 10.1007/s00256-023-04459-5
Norisyam Y, Shanmugam JT, Lim HS, Bahrin Z. Successful Empirical Treatment of Suspected Spinal Tuberculosis: A Case Report. Cureus. 2024 Mar 5;16(3):e55562. DOI: 10.7759/cureus.55562
Jung NY, Jee WH, Ha KY, Park CK, Byun JY. Discrimination of Tuberculous Spondylitis from Pyogenic Spondylitis on MRI. AJR Am J Roentgenol. 2004 Jun;182(6):1405-10. DOI: 10.2214/ajr.182.6.1821405
Panico CT, de Oliveira PRD, de Carvalho VC, Dos Anjos AM, de Melo VFA, Lima ALLM. Clinical-epidemiological profile of confirmed cases of osteoarticular tuberculosis. J Bone Jt Infect. 2023 Jan 5;8(1):11-7. DOI: 10.5194/jbji-8-11-2023
Nahid P, Dorman SE, Alipanah N, Barry PM, Brozek JL, Cattamanchi A, et al. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: Treatment of Drug-Susceptible Tuberculosis. Clin Infect Dis. 2016 Oct 1;63(7):e147-e95. DOI: 10.1093/cid/ciw376
Gupta S, Sinha U, Raj A. Severe Paradoxical Manifestations in an Immunocompetent Young Female With Tuberculous Meningitis. Cureus. 2022 Oct;14(10):e29953. DOI: 10.7759/cureus.29953
Dash N, Manion M, Silverberg SL, Kitai I. Identification and Management of Paradoxical Reactions in Pediatric Tuberculosis. Pediatr Infect Dis J. 2025 Mar 14. DOI: 10.1097/INF.0000000000004805
Kalita J, Shukla R, Pandey PC, Singh V, Haldar R, Misra UK. mRNA profiling of cytokines to understand paradoxical response in HIV-uninfected tuberculous meningitis. Tuberculosis (Edinb). 2024 Jan;144:102463. DOI: 10.1016/j.tube.2023.102463
Bell LC, Breen R, Miller RF, Noursadeghi M, Lipman M. Paradoxical reactions and immune reconstitution inflammatory syndrome in tuberculosis. Int J Infect Dis. 2015 Mar;32:39-45. DOI: 10.1016/j.ijid.2014.12.030
Geri G, Passeron A, Heym B, Arlet JB, Pouchot J, Capron L, et al. Paradoxical reactions during treatment of tuberculosis with extrapulmonary manifestations in HIV-negative patients. Infection. 2013 Apr;41(2):537-43. DOI: 10.1007/s15010-012-0376-9
Velivela K, Rajesh A. Paradoxical response in spinal tuberculosis: Lessons learnt. J Neurosci Rural Pract. 2016 Apr/Jun;7(2):206-9. DOI: 10.4103/0976-3147.178659
Pepper DJ, Marais S, Maartens G, Rebe K, Morroni C, Rangaka MX, et al. Neurologic manifestations of paradoxical tuberculosis-associated immune reconstitution inflammatory syndrome: a case series. Clin Infect Dis. 2009 Jun 1;48(11):e96-107. DOI: 10.1086/598988
Arifin J, Biakto KT, Johan MP, Anwar SFZ. Clinical outcomes and surgical strategy for spine tuberculosis: a systematic review and meta-analysis. Spine Deform. 2024 Mar;12(2):271-91. DOI: 10.1007/s43390-023-00785-9
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Infections in Evidence

This work is licensed under a Creative Commons Attribution 4.0 International License.
The Copyright Transfer Agreement also understands that the authors guarantee that the respective Case Report has never been published in another communication vehicle or scientific journal. Papers presented at meetings and/or scientific congresses may be published in the electronic Journal INFECTIONS IN EVIDENCE - Case Reports, provided they have not been published in whole or in part in their Proceedings or Annals in the format of a complete article including images, discussion and bibliographic references, or that they have not been assigned a specific DOI number.
















