Nephrectomy caused by Proteus mirabilis in a patient without clinical signs of sepsis
DOI:
https://doi.org/10.5935/2764-734X.e202112005Keywords:
Nephrolithiasis, Proteus mirabilis, PyonephrosisAbstract
A 40-year-old female patient due to pain in her abdomen for 3 days, not associated with urinary symptoms. There was a history of renal lithiasis without treatment 6 years ago. Physical examination did not show signs of sepsis, while computed tomography showed renal destruction. Nephrectomy was performed with Proteus mirabilis growed in culture. It has been known that this bacterium is associated to struvite stones, wich can cause pyonephrosis. Unortunately, the patient lost her kidney due to lack of adequate treatment.
Downloads
INTRODUCTION
Proteus mirabilis (PM) is a facultative anaerobic, Gram-negative bacterium of the Enterobacteriaceae family that is frequently associated with urinary tract infections1,2.
In addition to synthesizing virulence factors such as hemolysin, PM produces urease that hydrolyzes urea to ammonia and carbon dioxide2,3. In the presence of hydrogen, ammonia is converted into ammonium, thereby increasing the pH level of the urine. This alkalinization leads to phosphate and magnesium precipitation and the formation of struvite stones1,3. Such lithiasis results in a vicious cycle of increased bacterial proliferation, and consequently, increased urea and ammonium synthesis, urine alkalinization, and struvite precipitation2,4.
Struvite formation without adequate medical intervention generates an obstruction in the genitourinary tract, culminating in pyelonephritis1,5.
CASE DESCRIPTION
A 40-year-old, single, female post-graduate student presented to our department with severe abdominal pain associated with decreased stool clearance for three days.
The patient reported a history of renal colic associated with recurrent infections that started six years ago, but she has been in remission for two years already. During her follow-up session in the Department of Nephrology and Urology, a percutaneous nephrolithotripsy was scheduled; however, this was not performed due to covid-19 pandemic quarantine restrictions. There was no recent fever, decreased urine output, dysuria, and other urinary symptoms. She also denied tobacco smoking, alcohol drinking and had not undergone any previous surgeries.
Upon physical examination, she was afebrile, with a heart rate of 84 bpm and blood pressure of 140 ✕ 90 mmHg. She also had a palpable tumor of approximately 30 ✕ 20 cm on the right side, rebound tenderness, negative Giordano test, and a normal digital rectal examination.
The laboratory tests conducted at admission are outlined in Table 1.
| PATIENT | REFERENCE VALUES | |
|---|---|---|
| URINE | ||
| Leukocytes | > 1.000.000/ml | 0-10.000/mL |
| Nitrites | Positiveo | Negative |
| Red blood cells | 578 | 0-8.000/mL |
| Appearance | Purulent | Yellow |
| EXAMES SÉRICOS | ||
| C-reactive protein | 25,3 | Under 1mg/dL |
| Sodium | 134 | 137-145 mmol/L |
| Potassium | 4,4 | 3,5-5,1 mmol/L |
| Urea | 27 | 15-36 mg/dL |
| Creatinine | 0,8 | 0,53-1 mg/dL |
| Hemoglobin | 10,3 | 12-16 g/dL |
| Hematocrit | 30,7% | 36-46% |
| Serum leukocytes | 14.600 | 4.500-11.000/uL |
| Serum neutrophils | 83,9% (12.249) | 45,5-73,3% (1.600-7.700/uL) |
Contrast-enhanced computed tomography of the abdomen showed significant pyelocaliceal dilatation of the right kidney and the presence of kidney stones (Figures 1 and 2), leading to the diagnosis of pyonephrosis.
Figure 1. A large kidney stone on the renal pelvis.
Figure 2. Marked right kidney dilation with loculations indicative of pyonephrosis.
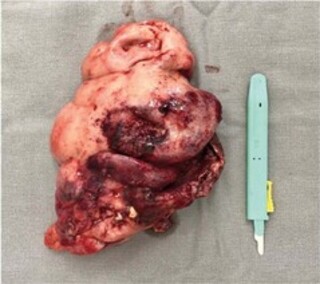
It was decided that a right subcapsular nephrectomy, with calyx draining, should be performed. During the surgery, a large amount of pus was found in the pyelocaliceal system. After removing the kidney (Figures 3 and 4), the urinary tract was reviewed for possible residual stones. Independent samples of kidney stone, kidney tissue, and pus were sent for culture and antibiogram (Table 2).
Figure 3. Right kidney (2.16 kg / 34.6 × 21.8 cm) showing pyonephrosis.
Figure 4. Struvite kidney stone measuring 6.4 × 5.8 cm.
| SAMPLE | BACTERIUM | SENSITIVITY | MIC (Minimum Inhibitory Concentration) | ANTIMICROBIAL RESISTANCE |
|---|---|---|---|---|
| Kidney stone | Proteus mirabilis | ≤8 | - | |
| Amikacin | ≤8 | |||
| Piperacilin/Tazobactam | ≤4 | |||
| Ampicillin | ≤1 | |||
| Aztreonam | ≤1 | |||
| Ceftazidime | ≤1 | |||
| Cefotaxime | ≤0,06 | |||
| Ciprofloxacin | ≤0,5 | |||
| Cefepime | ≤4 | |||
| Cefuroxime | ≤2 | |||
| Gentamicin | ≤0,5 | |||
| Levofloxacin | ≤0,12 | |||
| Meropenem sulfamethoxazole/ trimethoprim | ≤2/38 | |||
| Tobramycin | ≤2 | |||
| Fosfomycin | ≤16 | |||
| Renal parenchyma | Negative | - | - | - |
| Linezolid | ≤1 | Clindamycin | ||
| sulfamethoxazole / trimethoprim | ≤2/38 | Ciprofloxacin | ||
| Calyceal pus | Staphylococcus capitis | Teicoplanin | ≤1 | Erythromycin |
| Vancomycin | 1 | Gentamicin | ||
| Daptomycin | ≤1 | Levofloxacin | ||
| Fosfomycin | ≤32 | Oxacillin |
Postoperatively, the patient was clinically stable, afebrile, with clear diuresis, and no renal function deterioration. She was thus discharged from the hospital on the third postoperative day with instructions to continue taking 500 mg of cefuroxime every 12 hours.
DISCUSSION
Pyonephrosis is a urological emergency resulting from an infectious suppurative process during hydronephrosis. This causes renal parenchyma distortion or destruction, with possible loss of renal function. Pyonephrosis is usually associated with severe health impairment, including symptoms such as fever, chills, low back pain, and abdominal pain upon palpation2,6, 7, 8, 9.
Ultrasonography is a diagnostic method that is quite accurate and non-invasive. In this method, the lower portion of the dilated collecting system generates weak echoes and fluid levels. Excretory urography may be used to demonstrate hydronephrosis in non-functioning or severely compromised kidneys7,10,11. Computed tomography also helps in visualizing stones and identifying the degree of impairment of the renal parenchyma8,11,12.
It is common for patients with pyonephrosis to have a history of kidney stones and urinary tract infection that may be associated with the complete obstruction of the ureter7,8. The probability of having ureteral obstruction is exponentially greater in patients with stones larger than 5 mm and is almost certain with stones larger than 10 mm. It is thus important to consider whether the patient has a history of large stones7,8,10.
Pyonephrosis and urinary stasis brought about by ureteral obstruction predispose the patient to maintain and perpetuate a repetitive cycle of infection, which is worsened by the delay in treatment2,8,9. Even without a preventive solution through vaccination against PM12, patients with renal lithiasis should be monitored and treated carefully to avoid elevated levels of urease that may result in sepsis and kidney failure6.
Severe pyelonephritis is usually accompanied by thrombocytopenia, anemia, increased levels of transaminase, urea, and creatinine, resulting in acute renal failure. However, these were not observed in this patient, which may have contributed to the delay in diagnosis and treatment7,8,10,13.
Treatment is done by draining the infected renal pelvis and using broad-spectrum empirical antibiotic therapy. Percutaneous drainage is as effective as conventional surgery for the treatment of large and medium-sized renal abscesses. Pyonephrosis due to renal lithiasis can also be addressed by ureteroscopy7,8,10,14,15,16.
Delaying treatment may result in sepsis and a poor prognosis for renal viability, which may leave the patient with no other option but to undergo a nephrectomy6,8,9,14,15. In this case report, a nephrectomy was recommended due to total renal parenchyma destruction.
Histopathological examination of the resected kidney showed various degrees of renal parenchyma destruction, as well as dilatation of the pelvis and renal calyces. The increase in pressure resulting from the accumulation of purulent material further aggravated changes in the anatomical structure of the organ2,4,7.
Despite the long history of infection, the patient recovered satisfactorily after the kidney resection without serious complications such as septic shock, splenic abscess, psoas abscess, peritonitis due to rupture of the purulent collection, and renocolic fistulas8,13.
This case reports an atypical situation due to a nephrectomy performed in a patient with no general health impairment and afebrile throughout her infectious condition. Thus, physicians must investigate lithiasis associated with PM and carefully look for stones larger than 5 mm in women with recurrent urinary tract infections7,8,10.
“This case report deserved an official declaration of acknowledgement and ethical approval by its institution of origin and was peer-reviewed before publication, whilst the authors declare no fundings nor any conflicts of interest concerning this paper. It is noteworthy that case reports provide a valuable learning resource for the scientific community but should not be used in isolation to guide diagnostic or treatment choices in practical care or health policies. This Open Access artcle is distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work and authorship are properly cited.”
References
1. Armbruster CE, Mobley HLT, Pearson MM. Pathogenesis of Proteus mirabilis infection. EcoSal Plus. 2018 Feb;8(1):ESP0009.
2. Mobley HLT. Proteus mirabilis overview. Methods Mol Biol. 2019;2021:1-4.
3. Pearson MM. Culture methods for Proteus mirabilis. Methods Mol Biol. 2019;2021:5-13.
4. Allison C, Emödy L, Coleman N, Hughes C. The role of swarm cell differentiation and multicellular migration in the uropathogenicity of Proteus mirabilis. J Infect Dis. 1994;169(5):1155-8.
5. Norsworthy AN, Pearson MM. From catheter to kidney stone: the uropathogenic lifestyle of Proteus mirabilis. Trends Microbiol. 2017 Apr;25(4):304-15.
6. Li X, Lockatell CV, Johnson DE, Lane MC, Warren JW, Mobley HLT. Development of an intranasal vaccine to prevent urinary tract infection by Proteus mirabilis. Infect Immun. 2004 Jan;72(1):66-75.
7. Quhal F, Seitz C. Guideline of the guidelines: urolithiasis. Curr Opin Urol. 2021 Mar;31(2):125-9.
8. Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011 Mar;52(5):e103-20.
9. Xin J, Huang SD, Yu LX, Xin MH, Cai JS, Su ZJ. Pneumatic lithotripsy under ureteroscope for pyonephrosis due to calculus obstruction. Di Yi Jun Yi Da Xue Xue Bao. 2004 Oct;24(10):1199-20.
10. Jiang P, Xie L, Arada R, Patel RM, Landman J, Clayman RV. Qualitative review of clinical guidelines for medical and surgical management of urolithiasis: consensus and controversy 2020. J Urol. 2021 Apr;205(4):999-1008.
11. Romano J, Estrada C, Suárez N. Coraliform lithiasis. Aten Primaria. 2019 Aug/Sep;51(7):452-3.
12. Mahalingam H, Lal A, Mandal AK, Singh SK, Bhattacharyya S, Khandelwal N. Evaluation of low-dose dual energy computed tomography for in vivo assessment of renal/ureteric calculus composition. Korean J Urol. 2015 Aug;56(8):587-93.
13. Oka H, Nagamori T, Yamamoto S, Manabe H, Taketazu G, Mukai T, et al. Non-invasive discrimination of acute focal bacterial nephritis with pyelonephritis. Pediatr Int. 2019 Aug;61(8):777-80.
14. Chang CW, Huang CN. Pyonephrosis drained by double-J catheter. Clin Case Rep. 2020 Sep;8(12):3586-7.
15. Liu J, Chen L, An L, Ma K, Ye X, Xu Q, et al. Challenges and management of laparoscopic treatment of pyonephrosis caused by calculi. BMC Surg. 2020 Dec;20(1):327.
16. Florido C, Herren JL, Pandhi MB, Niemeyer MM. Emergent percutaneous nephrostomy for pyonephrosis: a primer for the on-call interventional radiologist. Semin Intervent Radiol. 2020 Mar;37(1):74-84.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Infections in Evidence

This work is licensed under a Creative Commons Attribution 4.0 International License.
The Copyright Transfer Agreement also understands that the authors guarantee that the respective Case Report has never been published in another communication vehicle or scientific journal. Papers presented at meetings and/or scientific congresses may be published in the electronic Journal INFECTIONS IN EVIDENCE - Case Reports, provided they have not been published in whole or in part in their Proceedings or Annals in the format of a complete article including images, discussion and bibliographic references, or that they have not been assigned a specific DOI number.
















