Multicentric Castleman disease in a patient infected with the human immunodeficiency virus
DOI:
https://doi.org/10.5935/2764-734X.e202205010Keywords:
Castleman Diseas, Lymphoma, AIDS-Related, Herpesvirus 8, Human, Systemic Inflammatory Response Syndrome, Sarcoma, KaposiAbstract
Castleman disease is a rare lymphoproliferative disorder with distinct clinical, histological and etiological presentations that may present as localized lymphadenopathy or systemic disease. The presentation of multicentric Castleman Disease is associated with human herpes virus-8, especially in patients infected with the human immunodeficiency virus and occasionally found with Kaposi’s Sarcoma. We present a case rarely described in the literature of a 41-year-old man with a recent diagnosis of human immunodeficiency virus infection and high viral load who developed peripheral lymph node enlargement associated with multicentric Castleman Disease and Kaposi’s Sarcoma after starting antiretroviral therapy.
Downloads
INTRODUCTION
First described in 1954 as a mediastinal and histopathological mass with hyperplastic lymphoid tissue and hyalinized germinal centers1, Castleman Disease (CD) currently refers to a group of different lymphoproliferative disease entities. The diagnosis is usually confirmed by lymph node histology, which can present three patterns: the hyalinevascular type, the plasma-cell type, and, more recently described, the multifocal plasmablastic type.
The extent of lymphadenopathy divides CD into unicentric (UCD) and multicentric (MCD). The hyaline-vascular type is mainly found in patients with UCD, while the plasmablastic type is common in patients with MCD, mainly in people living with HIV (PLHIV). The hyaline-vascular type usually involves systemic symptoms, multi-chain lymphadenopathy, splenomegaly, and often resembles hyperinflammatory disease or sepsis. The plasmablastic type progresses to a more aggressive disease, being initially described in the context of the POEMS (polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes) syndrome. Almost all MCD cases are HIV-associated, while about 50% of cases in HIV-negative patients are associated with human herpes virus-8 (HHV-8), which is also involved in the pathogenesis of Kaposi Sarcoma (KS)2. This may explain the frequent concomitance of KS and MCD, respectively described in 56% and 72% of PLHIV3,4. This association allows the overlap of another entity called Kaposi Sarcoma Inflammatory Cytokine Syndrome (KICS), which presents as a challenging differential diagnosis in the context of KS, MCD, and Immune Reconstitution Inflammatory Syndrome (IRIS)5.
CASE REPORT
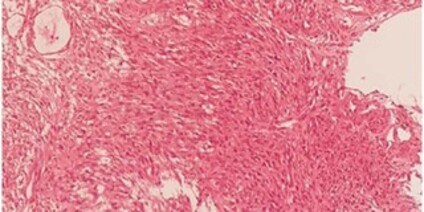
A single 41-year-old white man who had sex with men, civil police oficer, former smoker, diagnosed with HIV infection three months before. He had a viral load of 8,911,691 copies/ml, CD4+ T lymphocyte count of 214/mm3, and a CD4/CD8 ratio of 0.22. The patient was admitted with persistent symptoms including daily fever of 38º C, night sweats, productive cough, asthenia, and estimated weight loss of 6 kg (10% of body weight) over the last two months. Tenofovir, lamivudine, and dolutegravir have been used as antiretroviral therapy (ART) for 24 days, in addition to prednisone 20 mg due to anemia and thrombocytopenia evidenced at the time of HIV infection diagnosis. On physical examination, he had discolored mucous membranes; jaundice; palpable liver and spleen; and bilateral, painless and fibroelastic cervical, retroauricular, inguinal, and axillary lymph nodes. Serum tests showed hemoglobin 7.4 g/dL, platelet count of 43,000/mm3, leukocyte count of 3,700/mm3 (neutrophils, 1,700/mm3; lymphocytes, 1,600/mm3; and monocytes, 100/mm3), total bilirubin 3.17 mg/dL, direct bilirubin 2.5 mg/dL, C-reactive protein 174.4 mg/dL (RR < 5 mg/dL), and a new viral load of 3,065 copies/ml, CD4+ T lymphocyte count of 115, and CD4/CD8 ratio of 0.34. The diagnosis of IRIS associated with a possible lymphoproliferative neoplasm was considered, and corticotherapy and ART were maintained throughout the period. Abdomen computed tomography (CT) showed homogeneous hepatosplenomegaly without lymph node enlargement. Chest CT showed no abnormalities. Echocardiogram showed preserved ejection fraction and laminar pericardial efusion. The patient underwent bronchoscopy to collect bronchoalveolar lavage, which was negative for fungi and mycobacteria analysis and culture. Upper digestive endoscopy revealed edematous duodenal bulb inflammation and a velvety mucosa, whose biopsy revealed KS on pathological examination (Figure 1). Inguinal lymph node biopsy showed positive HHV-8 antigen immunohistochemistry and histological pattern with KS and CD components in the germinal center (Figures 2 and 3). Peripheral blood immunophenotyping identified B, T, and natural killer cell lymphopenia without anomalous lymphoid populations; myelogram showed hypocellular granulocytic and megakaryocytic series, meanwhile absolute hypercellularity at erythrocytic series. Clinically, the patient progressed with worsened hyperbilirubinemia and maintained thrombocytopenia and anemia, requiring blood component transfusion, in addition to renal dysfunction requiring hemodialysis. He also received several cycles of broad-spectrum antibiotic therapy and antifungal drugs throughout his prolonged hospital stay, beside empirical methylprednisolone pulse therapy for presumed hemophagocytic lymphohistiocytosis and foscarnet for cytomegalovirus infection. Chemotherapy was started with liposomal doxorubicin (a single dose); however, the patient progressed unfavorably with hemodynamic instability and died after 38 days of hospitalization.
Figure 1. Pathological analysis of gastric mucosa with typical spindle cells from Kaposi’s Sarcoma.
Figure 2. A. Reagent immunohistochemistry for HHV-8 in inguinal lymph node. Germinal center with infected lymphocytes; B. Reagent immunohistochemistry for HHV-8 in inguinal lymph node. Infected cells in a spindle-like pattern characteristic of Kaposi’s Sarcoma.
Figure 3. Pathological study of inguinal lymph node with hypervascular germinal center and lymphocytic depletion. Onion skinning in which lymphocytes from outside the mantle zone invaginate in concentric layers into the germinal center, characteristic of CD.
DISCUSSION
CD is a rare non-clonal lymphoproliferative disorder that can present as lymphadenopathy or disseminated disease. The simultaneous occurrence of MCD and KS in HIV-positive patients was first described by Lachant in 19856, and HHV-8 infection plays a central role in the pathogenesis of its disseminated form. Interleukin 6 (IL-6) from HHV-8-infected cells encodes a viral IL-6 (vIL-6) homolog that stimulates previously known human IL-6 (hIL-6)-induced signaling pathways, establishing a pro-inflammatory condition with significant systemic symptoms and increased acute phase reactants. Observational studies support the role of HHV-8 and vIL-6 expressed in lymph nodes of patients with CD, regardless of HIV serological status. In symptomatic patients with MCD associated with HHV-8, vIL-6 serum levels decrease according to treatment response and clinical improvement7.
Epidemiological data show that the incidence of HIV associated with MCD has been increasing in the era of highly active antiretroviral therapy (HAART)8, but whether the use of ART contributes to MCD onset or control in these cases is still uncertain. A review study including 84 patients with HIV infection associated with MCD showed that more than half of the patients had already received ART at the time of MCD diagnosis and 61.9% had an HIV viral load below 500 copies/mL3. Other data suggest that ART is beneficial, as in a series of seven HIV-positive patients on ART with a median survival of 36 months compared to 14 months in another study published before the systematic use of ART9. Some case reports describe HIV-positive patients with MCD who achieved full clinical and histological remission after using ART alone10, with resolution of constitutional symptoms within three months of initiating therapy11.
A more robust study with 24 patients proposed a relation between HHV-8 and HIV-associated MCD and suggested a higher risk of developing MCD in patients with a nadir CD4 greater than 200/mm3, known HIV infection of short duration, and no use of ART, which is rather contradictory regarding the risk of developing KS. Furthermore, HHV-8 DNA plasma levels were significantly higher with a diagnosis of MCD (median of 41,000 copies/ml) than of KS itself (median of 3,500 copies/ml)12.
Another cohort of patients with HIV infection associated with MCD showed a 15-fold increase in the incidence of non-Hodgkin’s Lymphoma (NHL), suggesting that the onset of MCD also increases the risk of NHL. Plasmablastic NHL is probably an expansion of MCD plasmablastic microlymphoma, whose multiclonal B-cell population may have an uncertain malignant capacity for developing an aggressive NHL13.
IRIS occurs in up to 30% of treatment-naive HIV-positive patients, and mortality ranges from 5% to 30%. In this syndrome, clinical deterioration may occur due to an aggravated known opportunistic infection or a neoplasm. On the other hand, the reconstitution of the host’s immune system can “unmask” a previously undiagnosed infection. The incidence of KS associated with IRIS reaches a variability of up to 30% between the populations studied, but there is insuficient evidence to associate MCD with IRIS, although case reports also describe episodes of acute worsening of MCD symptoms after ART10,14.
The relatively fast course of IRIS in our patient after three weeks of therapy can be explained by his treatment with an integrase inhibitor-based regimen (dolutegravir) whose high potency is recognized for increasing the chances of IRIS onset compared to other regimens, in addition to the fast viral load decrease and the low CD4+ T lymphocyte count at diagnosis, which are predictors of IRIS onset. Of patients with visceral KS, 16% developed IRIS-related KS, which had higher morbidity and mortality than IRIS caused by pneumocystosis, tuberculosis, and cytomegalovirus infection15.
Unlike IRIS associated with bacterial or fungal opportunistic pathogens, IRIS associated with KS should not be treated with steroids since they can accelerate HHV-8 replication and increase tumor growth16. Our patient received prednisone since HIV diagnosis, undergoing a three-day empirical methylprednisolone pulse therapy for hemophagocytic lymphohistiocytosis - this may have worsened KS associated with IRIS and MCD. Furthermore, worsened thrombocytopenia, anemia, and acute kidney failure are not findings compatible with IRIS associated with KS, but rather corroborate the hypothesis of severity caused by MCD. MCD mortality was around 44% in HIV-positive patients with HHV-8 in one study2 and two-year survival was 77.7% in another cohort12.
In 2010, a new IL-6-mediated IRIS entity was described in HIV-positive patients with HHV-8, which was called KICS3. Although these patients had the same clinical characteristics and laboratory tests that patients with MCD, bone marrow, spleen, or lymph node biopsies rule out MCD. This severe IRIS presentation has been postulated to be driven by a v-IL6, hIL-6, and h-IL10 cytokine storm encoded by HHV-817. In addition, IL-6 contributes to HHV-8 replication and KS progression, inducing B-cell proliferation and signaling increased vascular endothelial growth factor (VEGF) expression to promote typical KS angiogenesis. Patients with KICS have higher mortality rates than those with MCD, with fast clinical deterioration and death16.
The lack of treatment response in HIV-positive patients with MCD requires additional chemotherapy, with the most commonly used regimens being similar to those used for NHL: CVAD (cyclophosphamide, vincristine, doxorubicin, and dexamethasone), CHOP (cyclophosphamide, vincristine, doxorubicin, and prednisone), and ABV (doxorubicin, bleomycin, and vincristine). Treatment modalities for MCD and KICS are similar, but often, as illustrated in our case, patients are too severely ill to tolerate chemotherapy, with high mortality due to the overlap of MCD and KICS.
The combination of rituximab and doxorubicin has been used successfully since rituximab targets the cytokine-producing B cells that contain HHV-8 and doxorubicin helps eliminate KS spindle cells and prevents the aggressive KS proliferation that may occur in monotherapy18. A retrospective analysis of 52 HIV-positive patients with MCD showed a higher percentage of sustained remission and survival in patients receiving rituximab-based therapies compared to cytostatic therapy alone. A disadvantage of using rituximab seems to be a KS exacerbation in patients previously diagnosed with KS despite the concomitant use of ART19.
CONCLUSION
Despite the well-established definitions of CD, there is still a lack of more robust data on the therapy for HIV-positive patients with aggressive MCD, which has a poor prognosis and high mortality rate. This case report shows that MCD-associated HIV infection should be treated as a medical emergency, albeit a rare one. There is no correlation with CD4+ T lymphocyte count or previous use of ART and, given its heterogeneity and nonspecific clinical presentation, the diagnosis depends on high suspicion, with excisional lymph node biopsy and histological analysis by experienced pathologists being essential. Limitations in the management of this patient included the unavailability of vIL-6 dosage and the use of rituximab as an additional therapy. Further studies might suggest the need for monitoring HHV-8 infection in HIV-positive patients, thus valuing predictive signs of associated diseases.
“This case report deserved an official declaration of acknowledgement and ethical approval by its institution of origin and was peer-reviewed before publication, whilst the authors declare no fundings nor any conflicts of interest concerning this paper. It is noteworthy that case reports provide a valuable learning resource for the scientific community but should not be used in isolation to guide diagnostic or treatment choices in practical care or health policies. This Open Access artcle is distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work and authorship are properly cited.”
References
1. Cabot RC, Founder BC, Town VW. Case records of the Massachusetts general hospital weekly clinicopathological exercises: case 40011. N Engl J Med. 1954 Jan;250(1):26-30. DOI: https://www.nejm.org/doi/full/10.1056/NEJM195401072500107
2. Haq IU, Pria AD, Papanastasopoulos P, Stegmann K, Bradshaw D, Nelson M, et al. The clinical application of plasma Kaposi sarcoma herpesvirus viral load as a tumour biomarker: results from 704 patients. HIV Med. 2016 Jan;17(1):56-61.
3. Mylona EE, Baraboutis IG, Lekakis LJ, Ourania G, Papastamopoulos VV, Skoutelis A. Multicentric Castleman’s disease in HIV infection: a systematic review of the literature. AIDS Rev. 2008 Jan/Mar;10(1):25-35.
4. Oksenhendler E, Boutboul D, Fajgenbaum D, Mirouse A, Fieschi C, Malphettes M, et al. The full spectrum of Castleman disease: 273 patients studied over 20 years. Br J Haematol. 2018 Jan;180(2):206-16.
5. Uldrick TS, Wang V, O’Mahony D, Aleman K, Wyvill KM, Marshall V, et al. An interleukin-6-related systemic inflammatory syndrome in patients co-infected with Kaposi sarcoma-associated herpesvirus and HIV but without Multicentric Castleman disease. Clin Infect Dis. 2010 Ago;51(3):350-8.
6. Lachant NA, Sun NC, Leong LA, Oseas RS, Prince HE. Multicentric angiofollicular lymph node hyperplasia (Castleman’s disease) followed by Kaposi’s sarcoma in two homosexual males with the acquired immunodeficiency syndrome (AIDS). Am J Clin Pathol. 1985 Jan;83(1):27-33.
7. Aoki Y, Tosato G, Fonville TW, Pittaluga S. Serum viral interleukin-6 in AIDS-related multicentric Castleman disease. Blood. 2001 Abr;97(8):2526-7.
8. Bower M, Newsom-Davis T, Naresh K, Merchant S, Lee B, Gazzard B, et al. Clinical features and outcome in HIV-associated multicentric Castleman’s disease. J Clin Oncol. 2011 Jun;29(18):2481-6.
9. Aaron L, Lidove O, Yousry C, Roudiere L, Dupont B, Viard J. Human herpesvirus 8-positive Castleman disease in human immunodeficiency vírus-infected patients: the impact of highly active antiretroviral therapy. Clin Infect Dis. 2002 Out;35(7):880-2.
10. Zietz C, Bognor JR, Goebel FD, Löhrs U. An unusual cluster of cases of Castleman’s disease during highly active antiretroviral therapy for AIDS. N Engl J Med. 1999 Jun;340(24):1923-4.
11. Lee SM, Edwards SG, Chilton DN, Ramsay A, Miller RF. Highly active antiretroviral therapy alone may be an effective treatment for HIV-associated multicentric Castleman’s disease. Haematologica. 2010;95(11):1979-81.
12. Powles T, Stebbing J, Bazeos A, Hatzimichael E, Mandalia S, Nelson M, et al. The role of immune suppression and HHV-8 in the increasing incidence of HIV-associated multicentric Castleman’s disease. Ann Oncol. 2009 Abr;20(4):775-9.
13. Oksenhendler E, Boulanger E, Galicier L, Ming-Qing D, Dupin N, Diss TC, et al. High incidence of Kaposi sarcoma-associated herpesvirus-related non-Hodgkin lymphoma in patients with HIV infection and multicentric Castleman disease. Blood. 2002 Abr;99(7):2331-6.
14. Bottieau E, Colebunders R, Schroyens W, Van Droogenbroeck J, Droogh E, Depraetere K, et al. Multicentric Castleman’s disease in 2 patients with HIV infection, unresponsive to antiviral therapy. Acta Clin. 2000;55:97-101.
15. Goncalves PH, Ziegelbauer J, Uldrick TS, Yarchoan R. Kaposi sarcoma herpesvirus-associated cancers and related diseases. Curr Opin HIV AIDS. 2017 Jan;12(1):47-56.
16. Guo WX, Antakly T, Cadotte M, Kachra Z, Kunkel L, Masood R, et al. Expression and cytokine regulation of glucocorticoid receptors in Kaposi’s sarcoma. Am J Pathol. 1996 Jun;148(6):1999-2008.
17. Polizzotto MN, Uldrick TS, Wyvill KM, Aleman K, Marshall V, Wang V, et al. Clinical features and outcomes of patients with symptomatic Kaposi Sarcoma Herpesvirus (KSHV)-associated inflammation: Prospective characterization of KSHV inflammatory cytokine syndrome (KICS). Clin Infect Dis. 2016 Mar;62(6):730-8.
18. Uldrick TS, Polizzotto MN, Aleman K, Wyvill KM, Marshall V, Whitby D, et al. Rituximab plus liposomal doxorubicin in HIV infected patients with KSHV-associated multicentric Castleman disease. Blood. 2014 Dez;124(24):3544-52.
19. Hofmann C, Schmid H, Müller M, Teutsch C, Van Lunzen J, Esser S, et al. Improved outcome with rituximab in patients with HIV-associated multicentric Castleman disease. Blood. 2011 Set;118(13):3499-503
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Infections in Evidence

This work is licensed under a Creative Commons Attribution 4.0 International License.
The Copyright Transfer Agreement also understands that the authors guarantee that the respective Case Report has never been published in another communication vehicle or scientific journal. Papers presented at meetings and/or scientific congresses may be published in the electronic Journal INFECTIONS IN EVIDENCE - Case Reports, provided they have not been published in whole or in part in their Proceedings or Annals in the format of a complete article including images, discussion and bibliographic references, or that they have not been assigned a specific DOI number.
















