Lactobacillus species endocarditis in an immunocompetent patient
DOI:
https://doi.org/10.5935/2764-734X.e20230829Keywords:
Subacute bacterial endocarditis, Lactobacillus, Antibiotics, Penicillin, Cardiac surgical procedures, Case reportAbstract
Lactobacillus are gram-positive, facultative or strictly anaerobic bacilli commonly found in the gastrointestinal and female genital tracts and are rare human pathogens. This report presents a rare case of infective endocarditis caused by a Lactobacillus species in a patient with no known immunodeficiency. After the patient presented with a subacute fever and symptoms of heart failure, echocardiography was performed, which revealed a growth on the mitral valve. Further, blood cultures taken at admission indicated the growth of Lactobacillus casei/paracasei/rhamnosus in all samples. The minimum inhibitory concentration of penicillin for the agent identified was 0.38 mg/L. The patient was treated with beta-lactam monotherapy for 6 weeks, followed by elective surgical removal of the affected valve component. Finally, patient’s condition progressed with good clinical response, no complications, and no recurrence of symptoms 45 days after discharge.
Downloads
INTRODUCTION
Lactobacillus are gram-positive, facultative or strictly anaerobic bacteria with a bacilliform shape. Moreover, they are commensal organisms commonly found in the gastrointestinal tract, female genital tract, and oral cavity1,2. Some of these bacteria, such as L. paracasei and L. casei, have been used in probiotic foods and have been proven to be useful in the management of conditions such as vaginal candidiasis and diarrhea3. Although these bacteria are rare human pathogens, they can lead to serious conditions such as bacteremia, endocarditis, and intra-abdominal infections (including liver or splenic abscesses). These clinically significant infections have been associated with serious comorbidities (e.g., diabetes, cancer, and immunodeficiency), use of injectable drugs, prolonged use of antibiotics, and history of recent surgeries and dental procedures. Meanwhile, endocarditis is typically related to structural heart disease4,5. In this report, we present a rare case of infective endocarditis (IE) caused by Lactobacillus in a patient without severe comorbidities or known immunodeficiency.
CASE REPORT
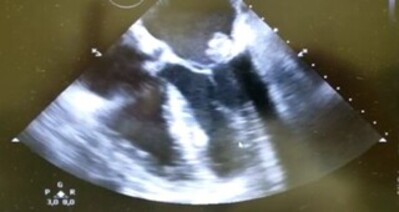
A 54-year-old man with a history of severe paranoid schizophrenia (rendering him legally incompetent while depending on help for basic life activities) was admitted to a public emergency room specializing in heart disease. He had lost 17 kg in the previous three months and had anorexia, episodes of fever (temperature up to 39°C) and bouts of night sweating. Moreover, he presented with dyspnea that had been progressively worsening for approximately one month along with lower-limb edema. The patient and his companion denied any history of smoking, alcoholism, or use of other drugs, but reported a history of undergoing saphenectomy in the previous year. On admission, his blood pressure was normal, and his heart rate was 80 bpm. His extremities were warm and well-perfused, and he had slight edema of the lower limbs. On auscultation, his heartbeat was rhythmic, with a systolic murmur (3+/6+) most audible at the mitral focus. His physical examination revealed no other remarkable changes. Initial laboratory tests indicated anemia, with hemoglobin levels of 8.1 mg/dL, and slightly elevated C-reactive protein levels at 7.7 mg/dL (reference value: 1 mg/dL). However, there were no other significant changes based on laboratory findings. The patient’s companion reported that the examination of the patient’s condition was already started by a private cardiologist, who ordered a transthoracic echocardiogram. This report noted “mitral valve thickening with prolapse of the anterior cusp and valve flail, indicating significant eccentric regurgitation, and a mobile echogenic image on the atrial surface of the anterior cusp, suggesting bacterial vegetation”. Further, a transesophageal echocardiogram obtained on the day after the patient’s admission confirmed these findings, revealing multiple hyperechoic, irregular, and mobile images at the mitral valve cusps, the largest of which measured 7 × 31 mm in its greatest diameter, suggesting bacterial vegetation. Despite the patient’s clinical stability, the medical team opted for an empirical prescription of ceftriaxone, oxacillin, and gentamicin, with plans to re-evaluate the regimen after obtaining the results of blood cultures. After hospitalization, the patient experienced sporadic fever spikes, with the last record of fever (axillary temperature of 38°C) obtained approximately 48 hours after the introduction of antimicrobials. The fever subsided thereafter. On the 4th day of hospitalization, all five blood culture samples (three from the day of admission and two from the following day) revealed a growth of Lactobacillus casei/paracasei/rhamnosus. The minimum inhibitory concentration of penicillin for the agent identified was 0.38 mg/L. Subsequently, the treatment regimen was changed according to the antimicrobial sensitivity test and crystalline penicillin was prescribed as monotherapy at a dose suitable for IE. Notably, blood cultures taken 72 hours after the start of penicillin therapy no longer led to the growth of microorganisms. The patient remained hospitalized and continued to receive intravenous antibiotic therapy. Further, there was clinical improvement and no complications, and the patient remained afebrile until the 19th day of hospitalization, when he underwent surgical removal of the mitral valve and implantation of a biological prosthesis. Anatomopathological examination of the removed tissue revealed the persistence of focus of infection, indicating that the valve leaflet had fibrosis, hyalinization, foci of myxoid degeneration and neutrophilic exudation, and capillary proliferation. On the 11th day after surgery, the patient was discharged from hospital with oral amoxicillin (after suspension of intravenous crystalline penicillin), aiming to complete six weeks of antimicrobial treatment in total. Further, at an outpatient visit 45 days after discharge, the patient remained clinically stable and afebrile, with no new complaints or complications.
DISCUSSION
Although rare, Lactobacillus species can cause clinically significant and potentially fatal diseases. In the literature, L. rhamnosus and L. casei have been described as the most common causes of invasive disease in humans4. IE is caused by Lactobacillus species in less than 1% of cases5,6. Unlike the case presented in this report, underlying comorbidities such as cancer, diabetes mellitus, and recent surgery are found in most patients who develop IE due to Lactobacillus; moreover, these species can even be considered as markers of a serious and fatal underlying disease6,7.
Notably, Cannon et al.4 analyzed more than 240 cases of infections caused by Lactobacillus from the existing literature. In their study, approximately 30% of the infections were reported as IE, indicating that infective endocarditis is an important differential diagnosis in patients with persistently positive blood cultures for Lactobacillus, even those with less obvious clinical findings, given the indolent nature of the infectious conditions associated with these pathogens.
Lactobacilli are generally considered commensal organisms, but they have been known to have pathogenic potential for a long time. Experimental studies in animal models have demonstrated that some isolates of these species can adhere to cell-matrix proteins, such as in abnormal valve tissues8. Additionally, some virulence factors can help bacteria colonize and survive, for example, by the production of enzymes and induction of platelet aggregation, as observed in other experimental models9.
These infections usually enter the body through the oropharynx, gastrointestinal tract, and, less frequently, the female reproductive tract. Moreover, medical interventions such as dental manipulations, abdominal surgeries, or endoscopic procedures are important events that can trigger these infections7,10,11. However, in this case, there was no history of any previous procedure of this nature in the patient.
Although there is no consensus in the literature on the best option for treating IE caused by Lactobacillus, some studies recommend using combined therapy with high doses of penicillin or ampicillin along with aminoglycoside11,12,13. This recommendation is partly based on the ability of these pathogens to develop antibiotic tolerance and, more specifically, the ability of a bacterial population to survive transient exposure to antibiotics at concentrations that would normally be bactericidal10. One of the mechanisms underlying this phenomenon has been suggested to be the ability of lactobacilli to produce lactic acid and thus generate an acidic environment, consequently reducing the action of certain antibiotics (especially beta-lactams and aminoglycosides)14. Meanwhile, the benefits of using aminoglycosides in combination therapy are being increasingly questioned, mainly because of the adverse effects (including nephro- and ototoxicity) associated with this class of antimicrobials, which are sometimes irreversible11,15.
Our patient was treated with beta-lactam monotherapy and became afebrile 48 hours after starting antimicrobial therapy. Subsequently, the patient had negative blood cultures. Valve replacement surgery was performed owing to the size of the bacterial growth and valve dysfunction associated with the infection. Notably, a surgical approach is often required in the treatment of IE caused by Lactobacillus, and this approach has been used in up to half of the cases reported in the literature4,7,10. However, in the present case, the successful outcome was consistent with the data from the leading reviews on the subject, which describe the effectiveness of monotherapy with beta-lactam agents for a reasonable period (usually 4–6 weeks) along with the removal of the affected valve component whenever needed4,7,10,16.
CONCLUSION
This report indicates that although Lactobacillus species are often mistaken for contaminants in standard medical practice, their pathogenic potential should not be underestimated, even in patients who are considered immunocompetent and do not have relevant medical comorbidities, as in the present case. Moreover, the successful treatment of the patient in this report demonstrates that it is possible to individualize antimicrobial treatment of IE caused by Lactobacillus based on the results of antibiotic sensitivity tests and host characteristics, particularly when used in combination with surgical removal of the compromised valve.
References
1. Bourne KA, Beebe JL, Lue YA, Ellner PD. Bacteremia due to Bifidobacterium, Eubacterium or Lactobacillus; twenty-one cases and review of the literature. Yale J Biol Med. 1978 Sep/Oct;51(5):505-12.
2. Petrova MI, Lievens E, Malik S, Imholz N, Lebeer S. Lactobacillus species as biomarkers and agents that can promote various aspects of vaginal health. Front Physiol. 2015 Mar;6:81.
3. Alvarez-Olmos MI, Oberhelman RA. Probiotic agents and infectious diseases: a modern perspective on a traditional therapy. Clin Infect Dis. 2001 Jun;32(11):1567-76.
4. Cannon JP, Lee TA, Bolanos JT, Danziger LH. Pathogenic relevance of Lactobacillus: a retrospective review of over 200 cases. Eur J Clin Microbiol Infect Dis. 2005 Jan;24(1):31-40.
5. See JR, Czachor JS, Brown GR. Lactobacillus endocarditis: case report and literature review. Infect Dis Clin Prac. 2006;14(3):134-6.
6. Borriello SP, Hammes WP, Holzapfel W, Marteau P, Schrezenmeir J, Vaara M, et al. Safety of probiotics that contain lactobacilli or bifidobacteria. Clin Infect Dis. 2003 Mar;36(6):775-80.
7. Husni RN, Gordon SM, Washington JA, Longworth DL. Lactobacillus bacteremia and endocarditis: review of 45 cases. Clin Infect Dis. 1997 Nov;25(5):1048-55.
8. Harty DW, Patrikakis M, Hume EB, Oakey HJ, Knox KW. The aggregation of human platelets by Lactobacillus species. J Gen Microbiol. 1993 Dec;139(12):2945-51.
9. Harty DW, Oakey HJ, Patrikakis M, Hume EB, Knox KW. Pathogenic potential of lactobacilli. Int J Food Microbiol. 1994 Dec;24(1-2):179-89.
10. Grazioli-Gauthier L, Rigamonti E, Leo LA, Lucchini GM, Priore EL, Bernasconi E. Lactobacillus jensenii mitral valve endocarditis: case report, literature review and new perspectives. IDCases [Internet]. 2022; 27:e01401. Disponível em: https://www.sciencedirect.com/science/article/pii/ S2214250922000294?via%3Dihub
11. Brouqui P, Raoult D. Endocarditis due to rare and fastidious bacteria. Clin Microbiol Rev. 2001 Jan;14(1):177-207.
12. Bayer AS, Chow AW, Betts D, Guze LB. Lactobacillemia — report of nine cases: Important clinical and therapeutic considerations. Am J Med. 1978 May;64(5):808-13.
13. Griffiths JK, Daly JS, Dodge RA. Two cases of endocarditis due to Lactobacillus species: antimicrobial susceptibility, review, and discussion of therapy. Clin Infect Dis. 1992 Aug;15(2):250-5.
14. Sussman JI, Baron EJ, Goldberg SM, Kaplan MH, Pizzarello RA. Clinical manifestations and therapy of Lactobacillus endocarditis: report of a case and review of the literature. Rev Infect Dis. 1986 Sep/ Oct;8(5):771-6.
15. Lebeaux D, Fernández-Hidalgo N, Pilmis B, Tattevin P, Mainardi JL. Aminoglycosides for infective endocarditis: time to say goodbye?. Clin Microbiol Infec. 2020 Jun;26(6):723-8.
16. Oakey HJ, Harty DW, Knox KW. Enzyme production by lactobacilli and the potential link with infective endocarditis. J Appl Microbiol. 1995 Feb;78(2):142-8.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Infections in Evidence

This work is licensed under a Creative Commons Attribution 4.0 International License.
The Copyright Transfer Agreement also understands that the authors guarantee that the respective Case Report has never been published in another communication vehicle or scientific journal. Papers presented at meetings and/or scientific congresses may be published in the electronic Journal INFECTIONS IN EVIDENCE - Case Reports, provided they have not been published in whole or in part in their Proceedings or Annals in the format of a complete article including images, discussion and bibliographic references, or that they have not been assigned a specific DOI number.
















