Spontaneous Remission of Diffuse Large B-Cell Lymphoma in a Patient with AIDS
DOI:
https://doi.org/10.5935/2764-734X.e20250956Keywords:
Neoplasm Regression, Spontaneous, Large B-Cell, Diffuse, Lymphoma, AIDS-Related, Antiretroviral Therapy, Highly Active, Case ReportAbstract
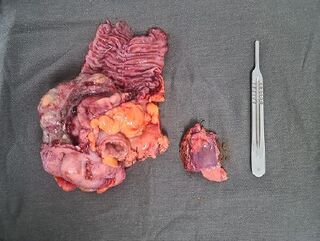
Diffuse large B-cell lymphoma (DLBCL) is the most common lymphoid hematologic neoplasm in adults living with HIV/AIDS. It is an aggressive disease, often with extranodal involvement, classically treated with chemotherapy. We report the case of a patient whose AIDS diagnosis was concomitant with an advanced lymphoma, requiring emergency intestinal resection due to an acute obstructive abdomen. Ten weeks postoperatively, spontaneous remission of the lymphoma was observed through positron emission tomography (PET/CT), a finding confirmed by a new surgical approach for intestinal transit reconstruction after six months and by a new PET/CT examination after one year. We attribute the phenomenon to immune reconstitution achieved through antiretroviral therapy and the associated use of ganciclovir for the treatment of cytomegalovirus infection.
Downloads
References
Dao A, Kim HY, Garnham K, Kidd S, Sati H, Perfect J, et al. Cryptococcosis: a systematic review to inform the World Health Organization Fungal Priority Pathogens List. Medical Mycology. 2024;62(6):myae043. doi:10.1093/mmy/myae043.
Kwon-Chung KJ, Bennett JE, Wickes BL, Meyer W, Cuomo CA, Wollenburg KR, et al. The case for adopting the “species complex” nomenclature for the etiologic agents of cryptococcosis. mSphere. 2017;2(1):e00357-16. doi:10.1128/mSphere.00357-16.
Speed B, Dunt D. Clinical and host differences between infections with the two varieties of Cryptococcus neoformans. Clinical Infectious Diseases. 1995;21(1):28–34. doi:10.1093/clinids/21.1.28.
Hamamoto Filho PT, Rodríguez-Rivas R, Fleury A. Neurocysticercosis: a review into treatment options, indications, and their efficacy. Research and Reports in Tropical Medicine. 2022;13:67–79. doi:10.2147/RRTM.S375650.
Kimura-Hayama ET, Higuera JA, Corona-Cedillo R, Chávez-Macías L, Perochena A, Quiroz-Rojas LY, et al. Neurocysticercosis: radiologic–pathologic correlation. Radiographics. 2010;30(6):1705–1719. doi:10.1148/rg.306105522.
Rosa-Júnior M, Cots E, Biasutti C. Teaching NeuroImage: cryptococcosis in the central nervous system mimicking neurocysticercosis. Neurology. 2022;98(12):e1302–e1303. doi:10.1212/WNL.0000000000200053.
Do Carmo FN, de Camargo Fenley J, Garcia MT, Rossoni RD, Junqueira JC, de Barros PP, et al. Cryptococcus spp. and cryptococcosis: focusing on the infection in Brazil. Brazilian Journal of Microbiology. 2022;53(3):1321–1337. doi:10.1007/s42770-022-00744-y.
Moretti ML, Resende MR, Lazéra MS, Colombo AL, Shikanai-Yasuda MA. Guidelines in cryptococcosis—2008. Revista da Sociedade Brasileira de Medicina Tropical. 2008;41(5):524–544. doi:10.1590/S0037-86822008000500022.
Trilles L, Lazéra MS, Wanke B, Oliveira RV, Barbosa GG, Nishikawa MM, et al. Regional pattern of the molecular types of Cryptococcus neoformans and Cryptococcus gattii in Brazil. Memórias do Instituto Oswaldo Cruz. 2008;103(5):455–462. doi:10.1590/S0074-02762008000500008.
Bartlett KH, Cheng PY, Duncan C, Galanis E, Hoang L, Kidd S, et al. A decade of experience: Cryptococcus gattii in British Columbia. Mycopathologia. 2012;173(5–6):311–319. doi:10.1007/s11046-011-9475-x.
DeBess E, Cieslak PR, Marsden-Haug N, Goldoft M, Wohrle R, Free C, et al. Emergence of Cryptococcus gattii—Pacific Northwest, 2004–2010. MMWR Morbidity and Mortality Weekly Report. 2010;59(28):865–868. Disponível em: https://www.cdc.gov/mmwr/pdf/wk/mm5928.pdf
Chen SC, Slavin MA, Heath CH, Playford EG, Byth K, Marriott D, et al. Clinical manifestations of Cryptococcus gattii infection: determinants of neurological sequelae and death. Clinical Infectious Diseases. 2012;55(6):789–798. doi:10.1093/cid/cis529.
Saijo T, Chen J, Chen SC, Rosen LB, Yi J, Sorrell TC, et al. Anti–granulocyte-macrophage colony-stimulating factor autoantibodies are a risk factor for central nervous system infection by Cryptococcus gattii in otherwise immunocompetent patients. mBio. 2014;5(2):e00912-14. doi:10.1128/mBio.00912-14.
Yang DH, England MR, Salvator H, Anjum S, Park YD, Marr KA, et al. Cryptococcus gattii species complex as an opportunistic pathogen: underlying medical conditions associated with the infection. mBio. 2021;12(5):e02708-21. doi:10.1128/mBio.02708-21.
Saidykhan L, Onyishi CU, May RC. The Cryptococcus gattii species complex: unique pathogenic yeasts with understudied virulence mechanisms. PLoS Neglected Tropical Diseases. 2022;16(12):e0010916. doi:10.1371/journal.pntd.0010916.
Setianingrum F, Rautemaa-Richardson R, Denning DW. Pulmonary cryptococcosis: a review of pathobiology and clinical aspects. Medical Mycology. 2019;57(2):133–150. doi:10.1093/mmy/myy086.
Howard-Jones AR, Sparks R, Pham D, Halliday C, Beardsley J, Chen SC. Pulmonary cryptococcosis. Journal of Fungi (Basel). 2022;8(11):1156. doi:10.3390/jof8111156.
Anjum S, Dean O, Kosa P, Magone MT, King KA, Fitzgibbon E, et al. Outcomes in previously healthy cryptococcal meningoencephalitis patients treated with pulse taper corticosteroids for post-infectious inflammatory syndrome. Clinical Infectious Diseases. 2021;73(9):e2789–e2798. doi:10.1093/cid/ciaa1901.
Liu J, Li M, Gan ZQ, Wang YJ, Lin CR, Chen ZL, et al. Postinfectious inflammatory response syndrome in HIV-uninfected and nontransplant men after cryptococcal meningitis. Future Microbiology. 2020;15:613–621. doi:10.2217/fmb-2019-0252.
Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clinical Infectious Diseases. 2010;50(3):291–322. doi:10.1086/649858.
Chang CC, Harrison TS, Bicanic TA, Chayakulkeeree M, Sorrell TC, Warris A, et al. Global guideline for the diagnosis and management of cryptococcosis: an initiative of the ECMM and ISHAM in cooperation with the ASM. The Lancet Infectious Diseases. 2024;24(8):e495–e512. doi:10.1016/S1473-3099(23)00731-4.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Infections in Evidence

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The Copyright Transfer Agreement also understands that the authors guarantee that the respective Case Report has never been published in another communication vehicle or scientific journal. Papers presented at meetings and/or scientific congresses may be published in the electronic Journal INFECTIONS IN EVIDENCE - Case Reports, provided they have not been published in whole or in part in their Proceedings or Annals in the format of a complete article including images, discussion and bibliographic references, or that they have not been assigned a specific DOI number.
















