Pericardite por Mycobacterium kansasii em pessoa vivendo com HIV
DOI:
https://doi.org/10.5935/2764-734X.e202205012Palavras-chave:
Pericardite, Mycobacterium kansasii, HIV, Relato de CasoResumo
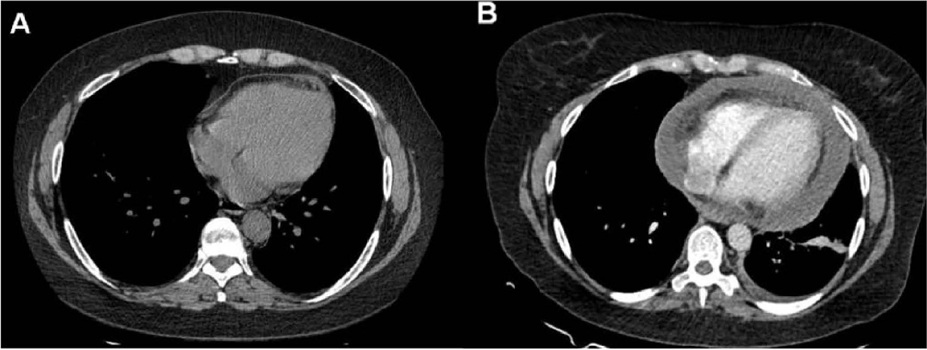
No que diz respeito à etiologia, a pericardite aguda por tuberculose é das mais prevalentes em nosso meio no contexto da aids. Neste trabalho relatamos o primeiro caso brasileiro com um surpreendente diagnóstico de pericardite por M. kansasii em função do levantamento tardio da cultura, destacando suas particularidades clínicas e laboratoriais (presuntivamente compatíveis com tuberculose), bem como as implicações terapêuticas deste resultado.
Downloads
Full-text of the article is available for this locale: English.
Referências
1. Vandi G, Calza L, Girometti N, Manfredi R, Musumeci G, Bon I, et al. Acute onset myopericarditis as unusual presentation of primary HIV infection. Int J STD AIDS. 2017 Fev;28(2):199-201. DOI: https://doi.org/10.1177/0956462416654852
2. Pham TV, Torres M. Human immunodeficiency virus infection-related heart disease. Emerg Med Clin North Am. 2015 Ago;33(3):613-22. DOI: https://doi.org/10.1016/j.emc.2015.04.009
3. Chiabrando JG, Bonaventura A, Vecchié A, Wohlford GF, Mauro AG, Jordan JH, et al. Management of acute and recurrent pericarditis: JACC state-of-the-art review. J Am Coll Cardiol. 2020 Jan;75(1):76-92. DOI: https://doi.org/10.1016/j.jacc.2019.11.021
4. Kytö V, Sipilä J, Rautava P. Clinical profile and influences on outcomes in patients hospitalized for acute pericarditis. Circulation. 2014 Out;130(18):1601-6. DOI: https://doi.org/10.1161/CIRCULATIONAHA.114.010376
5. Estok L, Wallach F. Cardiac tamponade in a patient with AIDS: a review of pericardial disease in patients with HIV infection. Mt Sinai J Med. 1998 Jan;65(1):33-9.
6. Gowda RM, Khan IA, Mehta NJ, Gowda MR, Sacchi TJ, Vasavada BC. Cardiac tamponade in patients with human immunodeficiency virus disease. Angiology. 2003 Jul/Ago;54(4):469-74. DOI: https://doi.org/10.1177/000331970305400411
7. Canelas C, Carvas JM, Fontoura JI, Lemos J. Pericarditis: not all are idiopathic. Galicia Clin. 2017;78(1):31-4.
8. Moreno F, Sharkey-Mathis PK, Mokulis E, Smith JA. Mycobacterium kansasii pericarditis in patients with AIDS. Clin Infect Dis. 1994 Nov;19(5):967-9.
9. Campo RE, Campo CE. Mycobacterium kansasii disease in patients infected with human immunodeficiency virus. Clin Infect Dis. 1997 Jun;24(6):1233-8.
10. Bacon ME, Whelan TV, Mahoney MD, Patel TG, Judson PL. Pericarditis due to Mycobacterium kansasii in a patient undergoing dialysis for chronic renal failure. J Infect Dis. 1985 Out;152(4):846-7.
11. Natori S, Morimoto H, Matsuzaki M, Matsuhashi H, Onodera S. A case of myelodisplastic syndrome with pericarditis due to atypical Mycobacterium. Nippon Kyobu Shikkan Gakkai Zasshi. 1994;32(1):101-5 apud Pintado V, Fortún J, Casado JL, Gómez-Mampaso E. Mycobacterium kansasii pericarditis as a presentation of AIDS. Infection. 2001 Jan/Fev;29(1):48-50.
12. Palmer JA, Watanakunakom C. Mycobacterium kansasii pericarditis. Thorax. 1984 Nov;39(11):876-7.
13. Pintado V, Fortún J, Casado JL, Gómez-Mampaso E. Mycobacterium kansasii pericarditis as a presentation of AIDS. Infection. 2001 Jan/Feb;29(1):48-50.
14. Cho JH, Yu CH, Jin MK, Kwon O, Hong KD, Choi JY, et al. Mycobacterium kansasii pericarditis in a kidney transplant recipient: a case report and comprehensive review of the literature. Transpl Infect Dis. 2012 Out;14(5):E50-5. DOI: https://doi.org/10.1111/j.1399-3062.2012.00767.x
15. Theodorou DJ, Theodorou SJ, Kakitsubata Y, Sartoris DJ, Resnick D. Imaging characteristics and epidemiologic features of atypical mycobacterial infections involving the musculoskeletal system. Am J Roentgenol. 2001 Fev;176(2):341-9.
16. Han SH, Kim KM, Chin BS, Choi SH, Lee S, Kim MS, et al. Disseminated Mycobacterium kansasii infection associated with skin lesions: a case report and comprehensive review of the literature. J Korean Med Sci. 2010 Jan;25(2):304-8. DOI: https://doi.org/10.3346/jkms.2010.25.2.304
17. Buhler VB, Pollak A. Human infection with atypical acid-fast organisms; report of two cases with pathologic findings. Am J ClinPathol. 1953 Abr;23(4):363-74 apud Johnston JC, Chiang L, Elwood K. 2017. Mycobacterium kansasii. Microbiol Spectr. 2017 Jan;5(1). DOI: https://doi.org/10.1128/microbiolspec.TNMI7-0011-2016
18. Johnston JC, Chiang L, Elwood K. Mycobacterium kansasii. Microbiol Spectr. 2017 Jan;5(1). DOI: https://doi.org/10.1128/microbiolspec.TNMI7-0011-2016
19. Manfredi R, Nanetti A, Valentini R, Ferri M, Morelli S, Calza L. Epidemiological, clinical and therapeutic features of AIDS-related Mycobacterium kansasii infection during the HIV pandemic: an 11-year follow-up study. HIV Med. 2004 Nov;5(6):431-6.
20. Montera MW, Mesquita ET, Colafranceschi AS, Oliveira Junior AC, Rabischoffsky A, Ianni BM, et. al. I Brazilian guidelines on myocarditis and pericarditis. Arq Bras Cardiol. 2013;100(4 Supl 1):1-36. DOI: https://doi.org/10.5935/abc.2013S004
21. Kutzner H, Argenyi ZB, Requena L, Rütten A, Hügel H. A new application of BCG antibody for rapid screening of various tissue microorganisms. J Am Acad Dermatol. 1998 Jan;38(1):56-60. DOI: https://doi.org/10.1016/s0190-9622(98)70539-0
22. Ministério da Saúde (BR). Secretaria de Vigilância em Saúde. Coordenação-Geral de Vigilância das Doenças de Transmissão Respiratória de Condições Crônicas. Manual de recomendações para o diagnóstico e tratamento das Doenças causadas por micobactérias não tuberculosas no Brasil. Brasília (DF): Ministério da Saúde; 2021.
23. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/ IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J RespirCrit Care Med. 2007 Fev;175(4):367-416.
24. Daley CL, Iaccarino JM, Lange C, Cambau E, Wallace RJ, Andrejak C, et al. Treatment of nontuberculous mycobacterial pulmonary disease: an official ATS/ERS/ESCMID/IDSA clinical practice guideline. Eur Respir J. 2020 Jul;56(1):2000535.
25. Dooley DP, Carpenter JL, Rademacher S. Adjunctive corticosteroid therapy for tuberculosis: a critical reappraisal of the literature. Clin Infect Dis. 1997 Out;25(4):872-87.
26. Isiguzo G, Bruyn ED, Howlett P, Ntsekhe M. Diagnosis and management of tuberculous pericarditis: what is new? Curr Cardiol Rep. 2020 Jan;22(1):2. DOI: https://doi.org/10.1007/s11886-020-1254-1
27. Marras TK, Daley CL. A systematic review of the clinical significance of pulmonary Mycobacterium kansasii isolates in HIV infection. J Acquir Immune Defic Syndr. 2004 Ago;36(4):883-9.
Downloads
Publicado
Como Citar
Edição
Seção
Licença
Copyright (c) 2022 Infectologia em Evidência

Este trabalho está licenciado sob uma licença Creative Commons Attribution 4.0 International License.
A Cessão de Direitos também entende que os autores garantem que o respectivo Relato de Caso nunca foi publicado em outro veículo de comunicação ou periódico científico. Trabalhos apresentados em reuniões e/ou congressos científicos podem ser publicados na Revista INFECTOLOGIA EM EVIDÊNCIA, desde que não tenham sido publicados total ou parcialmente em seus Anais no formato de um artigo completo incluindo imagens, discussão e referências bibliográficas, ou que lhes tenha sido atribuído um registro DOI específico.
















