Oral doxycycline as an alternative treatment for early neurosyphilis in a patient living with HIV
DOI:
https://doi.org/10.5935/2764-734X.e20240947Keywords:
Neurosyphilis, HIV infections, Doxycycline, Case reportAbstract
This report aims to describe the successful treatment using oral doxycycline for early neurosyphilis in a patient living with HIV, primarily presenting with skin lesions. The therapeutic proposal, chosen by the patient and based on UK medical guidelines, has not yet been validated by the Brazilian Ministry of Health. The treatment consisted of a single dose of penicillin G benzathine (2.4 million units) administered intramuscularly, followed by oral doxycycline (200 mg twice a day) for 28 days, with quarterly outpatient follow-up. The patient's symptoms resolved on the first visit, and the nontreponemal test (VDRL) in the cerebrospinal fluid was negative after 6 months. The current literature offers inconclusive results; however, this case suggests that oral doxycycline is a safe alternative for treating neurosyphilis in select cases, especially for patients with penicillin allergies, while providing the advantage of avoiding hospitalization.
Downloads
INTRODUCTION
Syphilis can be congenital or acquired, with the latter being divided into early or late1. These criteria are established based on the time elapsed between acquiring the infection and clinical manifestation or the detection of a reactive serological test result. Early syphilis includes the early latent (up to 1 year in duration, usually asymptomatic) and primary and secondary forms (progression of the primary infection). Late syphilis includes the late latent (lasting more than a year), tertiary forms and neurosyphilis1. Persistence of the infection in the central nervous system (CNS) leads to syphilitic meningitis, with early neurosyphilis defined as CNS involvement up to 2 years after primary infection2,3.
All patients with a reactive venereal disease research laboratory (VDRL) test in cerebrospinal fluid (CSF) should be treated for neurosyphilis, regardless of clinical signs or symptoms4. Other biochemical alterations in the CSF (even with a nonreactive VDRL test) and the concomitant presence of neurological, ocular, or otological signs and symptoms, or radiologic imaging characteristic of the disease in the CNS also warrant treatment4-6.
There is a higher incidence of neurosyphilis among people living with human immunodeficiency virus (PLHIV), and patients with a CD4 cell count of less than 350/mm3 are three times more likely to have neurological involvement3. However, the diagnosis of neurosyphilis in this group of patients is more challenging and controversial. European guidelines, for example, indicate that lumbar puncture should be performed on all PLHIV with late syphilis and a CD4+ count of ≤350 cells/mm3 (including those without neurological signs and symptoms) and/or those with a serum VDRL titer greater than 1:32 in the event of therapeutic failure after treatment for late syphilis5.
For all patients (including PLHIV) and clinical forms, syphilis treatment with penicillin is well established, with oral doxycycline emerging as an alternative option for the treatment of early and late syphilis, including in Brazil6. However, there are no data on the use of doxycycline in neurosyphilis in either the American7, European5, or Brazilian6 guidelines. The official recommendation for the treatment of neurosyphilis is intravenous crystalline penicillin G (3-4 million units every 4 hours or by continuous infusion for 14 days), and ceftriaxone (2 g a day for 10-14 days) is presented as the only alternative to penicillin in these three guidelines. The official UK guidelines8 are an exception in that they also include doxycycline as an alternative to parenteral penicillin for the specific treatment of neurosyphilis. Although this therapeutic option is not standardized in our country, it was used in the case reported herein, exemplifying a successful regimen of oral doxycycline in PLHIV with early neurosyphilis.
CASE REPORT
The patient was a 39-year-old heterosexual male from the interior of the state of Rio Grande do Sul, who had been living with HIV for 13 years. The consultation was prompted by the appearance of skin lesions 10 days before presentation, but he had been experiencing nausea and vomiting after meals for 30 days (for intermittent periods of 1-3 days), accompanied by dizziness, amaurosis, hand paresthesia, and an isolated episode of syncope. Ten days ago, erythematous spots appeared on his torso and progressed to his limbs, leading him to seek initial care at a basic health unit. There, he underwent a blood test that was positive for syphilis (VDRL titration of 1/16), a diagnosis that he linked to sexual exposure in a recent extramarital relationship. He had histories of anxiety and migraines as well as epilepsy as a result of a cryptococcoma diagnosed approximately 10 years ago. He was taking carbamazepine (200 mg three times a day), phenytoin (100 mg twice a day), escitalopram (10 mg twice a day), antiretroviral therapy for HIV (tenofovir 300 mg, lamivudine 300 mg, and dolutegravir 100 mg, the latter at a double dose due to the use of anticonvulsants), and fluconazole (150 mg three times a day) that was maintained continuously due to the recurrence of cryptococcosis after a previous attempt to discontinue the antifungal. The patient reported good adherence to treatment and outpatient appointments and progressed with a persistently undetectable HIV viral load and a last reported CD4+ cell count of 666/mm3. It was decided to prescribe penicillin G benzathine (a single intramuscular dose of 2.4 million units) and advise the patient to seek specialist assessment at the tertiary referral hospital where he was routinely monitored for his underlying disease. This consultation took place 5 days later, and the patient had new complaints during that time, such as odynophagia and lumbar pain radiating to the trapezius muscles. He did not report fever, weight loss, or night sweats. On admission, he had erythematous, nonsquamous lesions on the trunk, abdomen, back, and medial region of the forearms, bilaterally. The remaining physical examinations showed no noteworthy alterations. His recent medical records included positive IgG results for toxoplasmosis and cytomegalovirus as well as nonreactive serologies for hepatitis B and C, Chagas disease, and HTLV. There was also a nonreactive VDRL test taken at the last visit, 4 months ago.
The patient underwent lumbar puncture for CSF collection, and the analysis showed normocellularity (5 cells), hypoglycorrhachia (64 mg/dL), normal proteinorrhachia (40 mg/dL), and VDRL reactivity (1/16). Based on this result, treatment for neurosyphilis with crystalline penicillin was indicated, but the patient refused hospitalization. The alternative treatment of ceftriaxone at a dose of 2 g/day was also declined, as it was deemed unfeasible to access in the patient’s city of origin. By mutual agreement between the medical team and patient, it was finally decided to prescribe oral doxycycline 200 mg twice a day for 28 days.
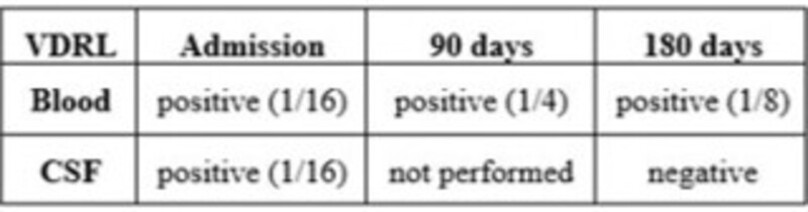
After a month of treatment, the patient returned for an outpatient visit reporting the disappearance of the spots on his skin and the complete resolution of his back pain, denying any other neurological, ocular, or otological signs or symptoms during the period. He returned after 3 months and remained asymptomatic. On this occasion, the control serum VDRL titration was 1/4 (a drop of two dilutions compared to the pretreatment test result). A new CSF sample was taken at the third appointment - 6 months after treatment - and the VDRL result was negative. He therefore returned to his regular consultations every 6 months due to his HIV infection. Table 1 summarizes the serum and CSF VDRL results over the period.
| VDRL | Pre-admission (120 days before) | Admission | 90 days | 180 days | |
|---|---|---|---|---|---|
| Blood | negative | positive (1/16) | positive (1/4) | positive (1/8) | |
| CSF | not performed | positive (1/16) | not performed | negative | |
DISCUSSION
All PLHIV diagnosed with syphilis should be assessed neurologically, and lumbar puncture is mandatory in the presence of neurological, ocular, or otological signs and symptoms5,6,8,9. In addition to its diagnostic importance, the nontreponemal VDRL test in the CSF serves as an important post-treatment monitoring indicator because a decrease in its titration is a sign of therapeutic success: a decline in the VDRL titration in the CSF greater than or equal to 4 times the initial value is expected 6-12 months after treatment for early neurosyphilis9,10. Normalization of serum VDRL levels combined with clinical response is also considered indicative of successful treatment of neurosyphilis7 because this blood result usually predicts normalization of the VDRL result in the CSF, especially in PLHIV undergoing antiretroviral therapy (as occurred in this case). However, some studies showed that this drop in titration was not observed in certain patients, especially elderly and female patients7,11.
The standard treatment for syphilis depends on the disease stage, while penicillin is used in almost all cases. Treponema pallidum is extremely susceptible to this antimicrobial due to its ability to block cell wall synthesis. Even after more than 60 years of clinical use, resistance has never been documented12. However, in some clinical situations (especially in allergic patients or in the event of a shortage)13, it is necessary to opt for alternatives to penicillin treatment. Most studies on this topic are small, uncontrolled, and retrospective, with tetracyclines being notable for their pharmacokinetic properties and greater bioavailability (more specifically doxycycline at a dose of 200 mg twice a day)5-7,9.
For neurosyphilis treatment, the primary objective is to ensure adequate antibiotic penetration across the blood-brain barrier. This requirement led to the use of crystalline penicillin instead of benzathine penicillin, which is typically used for other clinical forms of syphilis5-7,14. As an alternative or substitute, there is more robust evidence on ceftriaxone, which has been demonstrated to have an efficacy similar to penicillin G14. Meanwhile, the possibility of alternative oral treatment is particularly interesting and advantageous for neurosyphilis because both penicillin and ceftriaxone treatments require hospital care, which is not always available8,10.
Sufficient evidence supports the efficacy of doxycycline as a suitable alternative for treating early and latent neurosyphilis11. This has therefore been one of the official recommendations in the UK since 2015, as long as the patient is properly monitored through outpatient appointments at least every 3 months, including a reevaluation of the CSF at the end of 6 months of treatment8. In PLHIV, oral doxycycline may also be advantageous by reducing the risks associated with hospitalization, which can be elevated depending on the patient’s degree of immunodepression4.
Finally, it is worth noting that our patient received both an initial dose of benzathine penicillin and an additional 28-day course of oral doxycycline. Importantly, his main complaint was skin lesions, and benzathine penicillin is, by definition, the therapeutic recommendation for this secondary form of early syphilis. However, it was prescribed before the diagnosis of neurosyphilis; otherwise, the concomitant use of both treatments would not have been indicated. Conversely, considering that benzathine penicillin does not cross the blood-brain barrier, this double treatment cannot be considered a bias against the positive results obtained with doxycycline for the treatment of neurosyphilis, which is the main objective of this report15,16.
CONCLUSION
Oral doxycycline is not yet considered a validated option for the treatment of neurosyphilis in Brazil. Parenteral ceftriaxone is the only official alternative to penicillin; however, it’s use necessitates either a hospital stay or daily visits to a healthcare facility for administration.
This report of a successful case of treatment of neurosyphilis with doxycycline highlights the need for further studies into the efficacy and safety of this drug in the long term and confirms its practicality because it does not require the patient to be hospitalized.
“This case report deserved an official declaration of acknowledgement and ethical approval by its institution of origin and was peer-reviewed before publication, whilst the authors declare no fundings nor any conflicts of interest concerning this paper. It is noteworthy that case reports provide a valuable learning resource for the scientific community but should not be used in isolation to guide diagnostic or treatment choices in practical care or health policies. This Open Access article is distributed under the terms of the Creative Commons Attribution License (CC-BY), which allows immediate and free access to the work and permits users to read, download, copy, distribute, print, search, link and crawl it for indexing, or use it for any other lawful purpose without asking prior permission from the publisher or the author, provided the original work and authorship are properly cited.”
References
1. Avelleira JCR, Bottino G. Sífilis: diagnóstico, tratamento e controle. An Bras Dermatol. 2006;81(2):111-26. DOI: 10.1590/S0365-05962006000200002
2. Chan DJ. Syphilis and HIV co-infection: when is lumbar puncture indicated? Curr HIV Res. 2005;3(1):95-8. DOI: 10.2174/1570162052773031
3. Ceccarelli G, Borrazzo C, Lazzaro A, Innocenti GP, Celani L, Cavallari EN, et al. Diagnostic Issues of Asymptomatic Neurosyphilis in HIV-Positive Patients: A Retrospective Study. Brain Sci. 2019;9(10):278. DOI: 10.3390/brainsci9100278
4. Girometti N, Junejo MH, Nugent D, McOwan A, Whitlock G; 56 Dean Street Collaborative Group. Clinical and serological outcomes in patients treated with oral doxycycline for early neurosyphilis. J Antimicrob Chemother. 2021;76(7):1916-9. DOI: 10.1093/jac/dkab100
5. Janier M, Unemo M, Dupin N, Tiplica GS, Potočnik M, Patel R. 2020 European guideline on the management of syphilis. J Eur Acad Dermatol Venereol. 2021;35(3):574-88. DOI: 10.1111/jdv.16946
6. Brasil. Ministério da Saúde. Protocolo Clínico e Diretrizes para Atenção Integral às Pessoas com Infecções Sexualmente Transmissíveis [Internet]. Brasília: Ministério da Saúde; 2022; [Accessed in 2024 June 23]. Available from: http://antigo.aids.gov.br/pt-br/pub/2022/protocolo-clinico-e-diretrizes-terapeuticas-para-atencao-integral-pessoas-com-infeccoes
7. Workowski KA, Bachmann LH, Chan PA, Johnston CM, Muzny CA, Park I, et al. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm Rep. 2021;70(4):1-187. DOI: 10.15585/mmwr.rr7004a1
8. Kingston M, French P, Higgins S, McQuillan O, Sukthankar A, Stott C, et al. UK national guidelines on the management of syphilis 2015. Int J STD AIDS. 2016;27(6):421-46. DOI: 10.1177/0956462415624059
9. Qin J, Yang T, Wang H, Feng T, Liu X. Potential Predictors for Serofast State after Treatment among HIV-Negative Persons with Syphilis in China: A Systematic Review and Meta-Analysis. Iran J Public Health. 2015;44(2):155-69.
10. Li J, Zheng HY. Early syphilis: serological treatment response to doxycycline/tetracycline versus benzathine penicillin. J Infect Dev Ctries. 2014;8(2):228-32. DOI: 10.3855/jidc.3013
11. Peyriere H, Makinson A, Marchandin H, Reynes J. Doxycycline in the management of sexually transmitted infections. J Antimicrob Chemother. 2018;73(3):553-63. DOI: 10.1093/jac/dkx420
12. Lewis DA, Lukehart SA. Antimicrobial resistance in Neisseria gonorrhoeae and Treponema pallidum: evolution, therapeutic challenges and the need to strengthen global surveillance. Sex Transm Infect. 2011;87(Suppl 2):ii39-43. DOI: 10.1136/sti.2010.047712
13. Araujo RS, Souza ASS, Braga JU. Who was affected by the shortage of penicillin for syphilis in Rio de Janeiro, 2013-2017? Rev Saude Publica. 2020;54:109. DOI: 10.11606/s1518-8787.2020054002196
14. Bettuzzi T, Jourdes A, Robineau O, Alcaraz I, Manda V, Molina JM, et al. Ceftriaxone compared with benzylpenicillin in the treatment of neurosyphilis in France: a retrospective multicentre study. Lancet Infect Dis. 2021;21(10):1441-7. DOI: 10.1016/S1473-3099(20)30857-4
15. Clement ME, Okeke NL, Hicks CB. Treatment of Syphilis. JAMA. 2014;312(18):1905-17. DOI: 10.1001/jama.2014.13259
16. Ghanem KG, Erbelding EJ, Cheng WW, Rompalo AM. Doxycycline compared with benzathine penicillin for the treatment of early syphilis. Clin Infect Dis. 2006;42(6):e45-9. DOI: 10.1086/500406
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Infections in Evidence

This work is licensed under a Creative Commons Attribution 4.0 International License.
The Copyright Transfer Agreement also understands that the authors guarantee that the respective Case Report has never been published in another communication vehicle or scientific journal. Papers presented at meetings and/or scientific congresses may be published in the electronic Journal INFECTIONS IN EVIDENCE - Case Reports, provided they have not been published in whole or in part in their Proceedings or Annals in the format of a complete article including images, discussion and bibliographic references, or that they have not been assigned a specific DOI number.
















